
Shockwave Therapy For Tendon & Muscle Repair Treatments
Shockwave Therapy for Tendon Repair

Repetitive movements or actions often damage tendons, leading to chronic injuries. This is known as tendinopathy. It is estimated that 30% of consultations for musculoskeletal pain are related to tendinopathy, and 30-50% of sporting injuries involve tendinopathy. Statistical analysis reveals that the rotator cuff, Achilles, tibialis posterior, and patellar tendon are most prone to tendinopathy. Treatments are aimed at decreasing the pain and inflammation, then enhancing tissue repair and remodel.
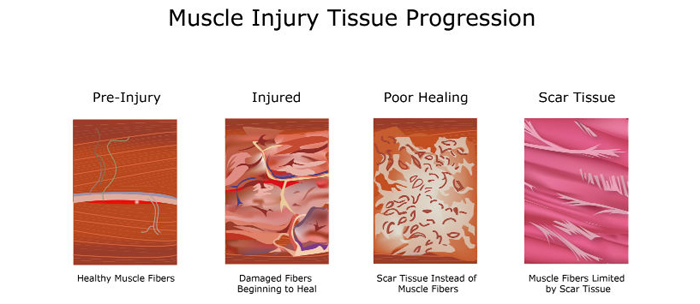
Shockwave therapy accelerates tendon healing and repair. It also causes the breakdown of scar tissue adhesions and conversion to proper tendon collagen. The treatment utilizes the body's natural healing and repair processes by causing micro damage to scar tissue and areas with chronic tendinopathy.
Shockwave therapy causes a very fast compression on the tissue, which effectively "stomps on the tissue." The sudden impact stretches the less flexible scar tissue and breaks it, triggering proper tissue repair. It produces a peak pressure over 1,000 times that of ultrasound waves to stimulate tissue repair and break up scar tissue. It is a very different treatment than ultrasound.
The treatment is not painful - much more comfortable than other treatments such as Graston Technique, ASTYM, or IASTM. These treatments also trigger tendon repair by activating the body's same tissue repair systems. Except Graston Technique and ASTYM utilize shearing and pulling across the scar tissue to tear it, which can cause bruising and excessive inflammation.
Video: Shockwave Therapy For Injuries
All of the treatments can help with tendon repair. We often use Graston Technique and shockwave therapy together to treat injuries. Shockwave therapy is commonly used first on very tender or painful injuries because it is more comfortably applied and produces less bruising and inflammatory response.

The intensity of shockwave therapy can be increased or decreased to make sure it is always comfortable. It should not hurt. Patients are often surprised that the comfortable compression can trigger the body's healing response. Those being treated with neck and back injuries frequently feel immediate relief and improved range of motion.
Many of our older patients prefer shockwave therapy to more aggressive soft tissue treatments because it causes less bruising and soreness post treatment, especially for those on blood thinners.
Before discussing how shockwave therapy enhances soft tissue repair, a review of anatomy and pathology helps to understand the condition and mechanism of repair.
What Is Tendinopathy
Tendinopathy is pain and reduced function of tendons. Often the injury is due to culmination of multiple pathological processes rather than a single event. The chronic repetitive stress leads to loss of tissue integrity and subsequent tearing or rupture.
I like to compare chronic repetitive injuries as adding pennies to a penny jar. Some days you add 15 pennies, some days you take out five pennies. Over time there is a tendency to add more pennies than you are removing, and eventually the jar starts to overflow. The overflowing penny jar is your chronic repetitive stress injury. There was not a single event or day that filled the jar; instead, the jar became full after an accumulation of days and pennies.

Often people are adding pennies to their jar because of muscle weakness, fatigue, or injury in other parts of their body. In addition to removing existing pennies from the jar, treatment will focus on reducing the amount of pennies you are adding every day.
The amount of repetitive stress placed upon your body can be dramatically reduced by changing postures and habits. For example, a person with low back pain may be uncomfortable sitting, which causes him to slouch at the computer. The slouching was contributing to neck pain and headaches. Improving the lower back pain will allow a person to sit with better posture and thus strain the neck less during the day.
Damage To Tendons
Mechanical and physical stress on tendons pull on the fibers. Too much pulling causes tears in the fibers, or even "fraying." Tendons will try and heal and repair, but cannot always completely finish repairing before the next trauma or physical stress.
Most Achilles tendon ruptures occur when participating in sporting activities. Often the ruptures are low grade damage has occurred. Biopsies have shown chronic degenerative changes in most ruptured Achilles tendons. These cases could be classified as acute trauma of chronically degenerated tendons.
In simple terms, the Achilles tendon has been chronically irritated with repetitive activity that has not completely healed, and then the Achilles ruptures during activity with a specific incident.

Repetitive loading and activity can be detrimental to tendon structures. The tendon repair mechanisms do not have enough time to heal before the onset of the next microtrauma or physical stress. This leads to a compromised tendon that is more susceptive to rupture.
Internal or intrinsic factors can make an individual more or less likely to suffer from a tendon injury. Factors include age, sex, and disease, such as diabetes, rheumatoid arthritis, ore genetic predisposition. Your overall health and condition can alter tendon structures or your ability to heal.
Muscle And Tendon Structure
The anatomical structure of muscles is like a licorice pull-and-peel. One fiber is wrapped in a group of fibers called a fascicle. Each fascicle is wrapped in a group of fascicles to form a muscle bundle. All the fibers are wrapped in coverings called fascia.
The coverings wrap around the individual fiber and the entire bundle. Each of the fascial coverings are a potential source of scar tissue formation, which will limit how the fiber slides and moves. This also changes the stress and strain that the muscle can handle.

This is the tendon, which is completely made of fascia and does not have any contractile properties like muscle. The muscles and fibers eventually end in a tendon that attaches to the bone. The muscle fascial coverings become thickened and dense before they attach to the bone.
Muscle contraction causes joint movement by pulling one bone closer to the other. Tendons transmit the forces produced by the muscles to the bone. The tendon is like a big thick rope; the tendon fibers are all aligned in the same direction to absorb the pulling forces.

Tendon fibers are made of type I collagen. This is a thick fiber designed to absorb and transmit forces. Excessive stress and strain in the fibers cause damage. Microtears in tendons are like nicking the fibers with a razor blade which cuts the fiber or causes it to fray. The body will try and repair this damage with proper type I collagen or it will form a temporary scar tissue patch with type III collagen.
In addition to chronic repetitive stress, microtears can be caused by uneven force production that results in uneven tendon loading. The amount of force absorbed by the tendon and the uneven distribution of forces lead to micro trauma and repair.
What are Scar Tissue And Fascial Adhesions?
Scar tissue forms when tissue does not heal correctly, or is under chronic repetitive stress. Scar tissue is weaker than normal muscle and connective tissue, which is why it becomes chronically sore with activity.
Scar tissue is like the body's duct tape; it is meant as a short term patch to help support tissue. However, in some cases the scar tissue is not replaced with normal type I collagen fibers. Instead, a weaker type III collagen is used as the duct tape.
Fascial adhesions are another term for scar tissue. Adhesions cause restrictions between the body's fascia. Stiffness, loss of normal range of motion and chronic pain develops from the type III collagen patches of fascial adhesions.
The next time a scar tissue patch undergoes stress and strain, it becomes aggravated and flares up. This process causes more scar tissue to be added to the outside of the patch and the process repeats itself over and over, leading to larger accumulation of scar tissue patches.
I like to describe these larger scar tissue patches as "onions." Scar tissue ends up growing in layers around the initial injury. Stress to the area aggravates the outside layers and triggers another layer to be formed. The layers further from the center are easier to aggravate than the inside layers, which is why the onion continues to grow in size without causing the inside area to properly repair.
Think of a chronic injury or area that bothers you. The same weak spot always flares up, weather it is in your low back, neck, or knee. The pain always seems to start in the same place over the years. This source of continued pain is a "scar tissue onion" or weak spot that keeps flaring up.
Causes of Scar Tissue
Four Common Causes of Scar Tissue
- Trauma- Sudden accident. Injuries like stepping off a curb or falling off a ladder.
- Repetitive Motion Injury- Same motion over and over.
- Improper Mechanics- Slouching at a computer makes muscles work harder to hold up your head, neck, and shoulders.
- Aging- Years of wear and tear on the body adds up.
In the end, any scar tissue that limits movement and causes pain needs to be broken up to restore normal motion.
That was the simple version.

A more complex and histological description of tendinopathy would include decreased oxygen and blood flow to the injured area. Tissue oxidative stress further decreases tissue repair and increases inflammatory cytokines. Tenocytes can produce substance P, catecholamines, glutamate, and acetylcholine.
Additional tissue repair cells play a role in tendon repair. Tenocytes within the tendon and sheath activate healing. Neutrophils and macrophages play a role in removing tissue debris and release chemicals that lead to the next phase of tissue repair.
The weaker scar tissue patch is made of type III collagen. In an ideal situation, the next repair phase transitions the type III to type I collagen, and this can continue for years beyond the original injury.
Is One Therapy Better Than Another For Chronic Tendinopathy?
No single therapy is consistently more effective than others.
Multiple therapies are often required for chronic tendinopathy repair and healing. We utilize shockwave therapy, Graston Technique, and class IV low level laser therapy to enhance tissue repair. Proper treatment and rehabilitation of tendinopathy injuries often requires incorporating exercises and stretches to increase muscle flexibility and strength. Then teaching the body how to use those muscles again properly. Muscle pattern and joint stability exercises can help prevent future injuries.