
Graston Technique Improves Lower Back Pain Treatments
Low Back Pain
Introduction and Causes of low back pain:
Low back pain is probably one of the most common medical complications affecting the lives of multiple people. A survey has shown that almost eighty percent of the US population experience lower back pain at some point in their life. Low back pain occurs in the lumbar region and sometimes, can be extremely intense. The most common causes of lower back pain are:
- Strain in the lumbar region.
- Lifting heavy weights and poor posture.
- Herniated discs, wear and tear of the cushioning discs between the vertebrae which act as shock absorbers.
- Degenerative disc disease.
- Injury to bones, ligaments or joints of the spinal cord.
ANATOMY OF LOWER BACK PAIN

Had our spinal cord been straight and rigid, we would have been stiff and unable to undertake any movements. Instead it is a coalition of multiple moving pieces which allow us to bend, rotate and twist. The lumbar spine is the portion of our spinal cord about five-six inches below the shoulder and extending up to the abdomen. It connects the thoracic spine and the sacral spine. In between each vertebrae are disc like structures which serve as shock absorbers and prevent them from grinding against each other. The discs can be thought of as doughnut having jelly like stuff inside called the nucleus pulposus. Wear and tear of the discs leads to squeezing out of the jelly from the discs which come in contact with the nerves and cause exhilarating pain.
Few common types of low back pain include axial pain (such as muscle strain), referred pain (like degenerative disc disease) and radicular pain (sciatica).
CONVENTIONAL MEDICATIONS OF LOWER BACK PAIN
The most commonly used medications for treating lower back pain includes acetaminophen, NSAIDs, oral steroids, narcotic drugs, muscle relaxants and antidepressants. The most widely used NSAIDs (non-steroidal anti-inflammatory drugs) are Ibuprofen, Naproxen, COX-2 inhibitors. In severe cases injections include epidurals and nerve blocks.
Graston Technique is utilized in many professional, Olympic, and collegiate sports therapy programs. Specifically-designed stainless steel instruments have rounded, concave and convex edges. The edges are not sharp. Graston tools are classified under Instrument Assisted Soft Tissue Mobilization (IASTM) and are used to detect and effectively treat soft tissue fibrosis or chronic inflammation. With these instruments the practitioner can scan over and detect areas of fibrotic tissue.
There are six different Graston tools to help break up fascial restrictions or scar tissue that develops after trauma to muscles, ligaments, tendons, or fascia, which is commonly referred to as soft tissue. Scar tissue forms when tissue does not heal correctly, or is under chronic, repetitive stress. Scar tissue is weaker than normal muscle and connective tissue, which is why it becomes chronically sore with activity.
What is Scar Tissue and Fascial Adhesion?
Scar tissue accumulates in the body whenever tissue undergoes excessive stress and strain. Scar tissue is like the body's duct tape; it is meant as a short term patch to help support tissue. However, in some cases the scar tissue is not replaced with normal collagen fibers. Scar tissue is also referred to as fascial adhesions, as it causes restrictions between the body's fascia. Stiffness, loss of normal range of motion and chronic pain develops from patches of fascial adhesions.
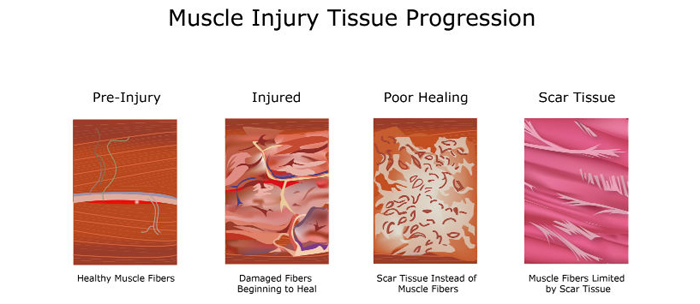
The next time a scar tissue patch undergoes stress and strain it becomes aggravated and flares up. This process causes more scar tissue to be added to the outside of the patch and the process repeats itself over and over, leading to larger accumulation of scar tissue patches.
I like to describe scar tissue patches as "onions." Scar tissue ends up growing in layers around the initial injury. Stress to the area aggravates the outside layers and triggers another layer to be formed. The layers further from the center are easier to aggravate than the inside layers, which is why the onion continues to grow in size without causing the inside area to properly repair.
Video: Scar Tissue Treatment with Graston Technique for Muscle Pain
How Graston Technique Improves Treatment
Adding Graston Technique to any treatment decreases overall treatment time. It reduces the need for anti-inflammatory medication and enhances rehabilitation. Many patients with chronic conditions show significant improvement with IASTM. Your provider is trained in how to properly utilize the instrument assisted soft tissue mobilization of either Graston, Gua Sha, and ASTYM. Basic concepts and treatments with IASTM:
- Reduce the stress and strain to the injured areas.
- Decrease inflammation.
- Increase muscle flexibility and strength.
- Increase blood flow.
- Break up scar tissue.
- Promote proper tissue repair.
- Enhance functional movements.
- Accelerate fibroblast activity.
Home therapies are recommended to limit further scar tissue formation, encourage proper healing and speed up recovery. Braces and supports may be recommended for specific injuries.
Pulling Fascia Apart to Break Up Scar Tissue
Graston Technique works by stretching the outer layer of the "onion" and breaking it into several pieces. The Graston instruments use shear force to pull the top fascial layer across the bottom fascial layer. This pulling motion breaks up the scar tissue between the layers. The broken scar tissue triggers healing mechanisms to migrate into the tissue and properly repair the muscles and soft tissues.
Ice therapy helps limit additional scar tissue formation, inflammation, and pain. The next office visits breaks up the next layer of scar tissue, working toward the center of the onion. The goal is to get to the center of the onion so the body can fix the original problem.
Many sports therapy chiropractors, physical therapists, doctors, and athletic trainers have been properly trained in how to utilize the Graston tools.
Expectations of Therapy
Graston Technique is not meant to be painful and should be performed at a comfortably tolerable level to break up scar tissue. Being too aggressive with Graston Technique, Active Release Technique, manual therapy, cross friction therapy, or massage therapy causes excessive pain and actually slows the repair process by flooding the area with inflammation.
Treatment usually lasts a few minutes per area or region. As the treatment tool slides across the soft tissue fibrotic areas, the injury may feel "bumpy or sandpaper-like." Redness and mild swelling may develop with treatment, especially after the first few treatments. In some cases, small petechiae or bruises may develop post-treatment. Ice therapy is commonly utilized post-treatment to limit the bruising, pain, and inflammation.
Most people notice a significant difference after 4-6 visits. Severe cases may take a little longer to see significant improvement. Runners, triathletes, and weekend warrior athletes have all benefited from this therapy. Over the course of treatment, most patients notice that less bumpiness, sandpaper, and tenderness is felt around the injury. As the treatment progresses, your healthcare provider will be able to apply more pressure, thereby treating deeper and deeper tissue levels.
Conservative Treatments Combined with Graston Technique
Therapeutic treatments for addressing soft tissue injuries involve massage therapy, manual therapy, trigger point therapy, or Active Release Technique combined with Graston Technique. These treatments increase blood flow, decrease muscle spasms, enhance flexibility, speed healing, and promote proper tissue repair.
When these treatments are incorporated into a treatment plan patients heal faster and are less likely to have long-term pain or soft tissue fibrosis or scar tissue in the injured muscle. These soft tissue treatments are integrated with therapeutic exercise and flexibility programs.
Soft tissue treatments restore proper muscle function and flexibility; and exercise restore strength, endurance, and neuromuscular control. Neuromuscular control is especially important and often not emphasised in many therapy clinics.
For any joint to work optimally the muscles need to contract and the exact right time. In many chronic injuries the muscles are not "firing" correctly leading to excessive strain on neighboring muscles and tendons. Many chronic rotator cuff injuries are the result of poor neuromuscular control.
Low back Injuries are commonly associated with poor joint stabilization in the foot, knee, or hip. This leads to poor alignment and excessive forces being placed onto muscles and tendons. Knee injuries and patella tendonitis are common with low back pain because of weakness and poor stabilization of the leg and hip muscles. Combination of muscle weakness, poor coordination, and altered gait mechanics place excessive stress on the knee, hip, and back. Knee pain treatments improve chronic knee and low back pain.
Your chiropractor, physical therapist, occupational therapist, or physician will evaluate your condition and make a proper diagnosis and treatment recommendations. Ask them any questions you might have about your injury.
Chiropractic Adjustments
Chiropractic manipulation treatments increase the movement of a joint complex. With injury, poor posture, sprains, and strains, muscles tighten up and the joints can become locked up. This lack of movement is felt when you can not look over your shoulder without feeling pulling, dull pain, or a twinge of pain. Mildly stuck joints can be loosened up in the day with stretching and range of motion exercises. Moderately stuck joints often need a little help to restore their normal motion with chiropractic adjustments.
Severely stuck joints cause a person pain whenever they put pressure upon the joint or try and move the joint complex.
There are multiple ways to get a joint moving again. The most important part is that the joint is moving in its proper range of motion and without pain. Many people think chiropractors only perform manual manipulation. Most likely their first experience with a chiropractic was years ago, and manual manipulation was the most common form of treatment. Over time and with technology, treatments have changed with the same goal of getting neck joints moving. Learn more about types of chiropractic adjustments.
Medical Treatments
NSAIDs are often prescribed for the initial acute injury stages. In severe cases that involve multiple joint regions, muscle relaxers or oral steroids can be given. Trigger point injections, botox, or steroid injections can be treatment options. Prolotherapy or Platelet Rich Plasma (PRP) Injection therapy can enhance healing, especially with internal joint injuries or difficult tendon injuries. Pain management is not usually required unless stronger medications or advanced joint injections are required for treatment.
MRI and X-rays will not usually be ordered to evaluate mild to moderate muscle, tendon, and ligament injuries. Severe cases may utilize advanced imaging to rule out bone fractures, edema, nerve entrapments, tendon or muscle ruptures. NCV testing may be utilized in cases that also involve muscle, sensory, or reflex loss.
Lumbar disc bulges and herniations onto the spinal cord or nerve root produce different symptoms and location of symptoms. Pain radiating in the foot is one symptom; along with numbness, weakness, fatigue, loss of sensation, or reduced reflexes. Your chiropractor, physical therapist, occupational therapist, or physician will evaluate your condition and make a proper diagnosis and treatment recommendations. Ask them any questions you might have about your injury.
Many people do have arthritis or degenerative changes in their back, hip, knee, or foot joints. Arthritis does not mean you will always have pain in the joints. Degenerative arthritis means the structural integrity of the bones have changed which alters its gliding, sliding, and hinging motions. The more severe the arthritic changes the easier it becomes to aggravate the joint and produce pain.
Likewise joints may take longer to heal when joints they have significant joint cartilage and bone degeneration. Osteoarthritis and rheumatoid arthritis will also slow healing and recovery time. However, arthritis does not mean a joint will always be painful. People with severe arthritis can eventually be pain free. In fact many times incorrectly blame their arthritis as the source of their pain when it is actually coming from injured tendons.
This is especially common in knee pain, where people believe their daily dull and sharp pain is osteoarthritis or meniscus tears when much of the pain is coming from chronic knee tendonitis in the small tendons that insert around the knee joint and patella bone. Graston Technique is especially effective at stimulating and enhancing tendon repair and eliminating chronic tendon pain.
Low level laser therapy is another treatment option for enhancing muscle and tendon healing. Class IV cold lasers stimulate the fibroblasts or healing cells to "work faster." Specific frequencies can also decrease inflammation in the soft tissues and inside of the joints. Combining low level laser therapy with Graston Technique enhances soft tissue healing and repair.
Graston Technique Enhances Treatment and Recovery
The low back and lower extremity works as a comprehensive unit so you can run, walk, squat, bend, or turn. You appreciate your legs when many basic and repetitive tasks at home, work, or the gym become impossible because of pain. Injuries to one area of the musculature often indicate that additional damage has been incurred by other muscles.
Many therapeutic exercises can help restore proper strength and endurance to the hip and leg muscles. Isometric exercises are often the initial treatment exercises. Followed by single plane rubber band exercises for flexion, extension, adduction, abduction, and rotational movements. Dynamic exercises involving stability ball, BOSU, Foam, and vibrational exercises enhance propioception and neuromuscular control. The more unstable of the surface the more effort and stabilization is required of all the low back and leg muscles.
Our Chandler Chiropractic and Physical Therapy Clinic treats patients with a variety of low back muscle, tendon, joint, and ligament injuries. The clinic provides a combination treatment from a variety of providers, including chiropractic, physical therapy, and massage therapy. We work with all ages and abilities of the residents in Phoenix, Tempe, Gilbert, Mesa, and Chandler AZ.