
Medial Epicondylitis (Golfer's Elbow) Treatments in Chandler
Golfer's Elbow Treatment in Chandler Arizona
If you are experiencing pain on the inside of your elbow that gets worse when you are swinging a golf club, throwing, playing tennis or lifting weights, the cause may be golfer's elbow or medial epicondylitis. Pain on the inside of the elbow isn't as common as tennis elbow (aka lateral epicondylitis), but it can be an aggravating and chronic problem. Early treatment prevents the condition from causing permanent damage to the flexor tendons in the forearm, which might need to be corrected surgically.

What is Golfer's Elbow
Golfer's elbow, also known as medial epicondylitis, is a repetitive stress or overuse injury that affects the flexor and pronator muscles and tendons of the forearm. The medial epicondyle is the bony protrusion on the inside of the elbow: the site where you typically experience the most pain.
Golfers may develop pain on the inside of the elbow from incorrect form ("hitting from the top"). Medial epicondylitis also affects bowlers, pitchers, javelin throwers, racquet sports players and football players. It is also associated with certain occupations such as carpentry and plumbing.
Although the condition is most often caused by overuse or improper form, it can also result from a direct hit to the area or sudden, extreme, eccentric contraction: something that might happen if you try to lift too much weight doing a biceps curl (the eccentric movement is the lowering of the weight).
Early on, you might notice some swelling in the area. This may subside with time, even if the condition persists (e.g. pain). Because these tendons are located near the ulnar nerve, you may also experience tingling in the arm or numbness.
Over time, the condition may also affect the medial collateral ligament that stabilizes your elbow during movement. Some pitchers also develop calcification and/or bone spurs in the area.
Golfer's Elbow Video
Symptoms of Golfer's Elbow
If you are experiencing any of the following symptoms, it's time to contact your chiropractor and/or physical therapist about golfer's elbow:
- Pain on the inside of the elbow that becomes worse with movement. The pain may radiate down the inside of the forearm. Although the pain may subside with rest, it resumes with the movements that caused the injury.
- Numbness or tingling due to involvement of the ulnar nerve.
- Swelling and tenderness in the area.
- Weakness in the hands or wrists, especially when flexing the muscles that control them.
- Over time, the condition can limit range of motion, especially for pitchers.
Who is at Risk for Golfer's Elbow?
Golfer's elbow affects men and women equally; prevalence is highest in the fourth and fifth decades of life. Younger athletes who compete at the elite and semi-elite levels may also be affected. Risk factors include:
- Participating in sports including golf, tennis, bowling, weight lifting, pitching and javelin throwing.
- Improperly fitted sports equipment, particularly grip size for golf clubs and tennis racquets.
- Certain types of manual labor including carpentry and plumbing.
- Obesity
- Smoking
Home Treatment for Golfer's Elbow
The first thing you need to do if you develop golfer's elbow is to stop the activity that led to the injury. We know this is tough for those who love getting out on the links during the Fall, Winter and Spring seasons in southern Arizona, but if you continue to play, you will continue to hurt.
Ice is your best friend. Apply an ice pack to the area 3-4 times per day.
Your primary care physician may recommend anti-inflammatory medications such as Advil, aspirin, Aleve or Tylenol for 10-14 days to reduce swelling in the area. He or she may also recommend a night splint.
Medial and Lateral Epicondylitis Video
Medical Treatments
If your pain and swelling doesn't respond to over-the-counter anti-inflammatory medications, your primary care provider may recommend a corticosteroid injection. The injection will decrease pain and inflammation and may help you to begin range of motion exercises earlier.
Simple Conservative Treatments
If home treatments don't resolve the problem, the next step is active treatments including physiotherapy. The physical therapist may use ultrasound or electric stimulation to decrease pain in the area.
Counterforce bracing can help you to complete activities of daily living without making the symptoms worse. Taping can also help.
Establishing full, painless range of motion is the first goal, before beginning exercises to strengthen the area. At the same time, it's important to continue with general condition exercises that target the core, muscles of the middle back and chest, to make sure that weaknesses in these areas aren't causing you to improperly use your forearm muscles.
Your physical therapist should evaluate your form if you became injured while playing a sport. Form errors include "throwing" from the apex of the backswing when playing golf, incorrect serving and forehand stroke for tennis players. Professional pitchers can develop muscle imbalances such as hypertrophy of the flexor forearm muscles that alter the valgus angle of the elbow and lead to medial epicondylitis.
Advanced Epicondylitis Treatments
Once the swelling and pain in the area has subsided and range of motion is restored, the next step is to strengthen weak muscles and correct muscle imbalances that may have led to the injury.
This is a case in which some is good, but more is not necessarily better. Start low and go slow when beginning to strengthen the injured muscles. Exercises may include rows, flies, curls, reverse curls, kickbacks, supination and pronation of the forearm, as well as lat raises (side and forward) and core exercises on the stability ball such as planks, glute bridging and mountain climbers to address any weakness in the hips, abdominal, lower and middle back muscles.
If you are a racquet sports player, exercises that develop agility in side-to-side motion are important so that you don't constantly over-reach to return balls. Along similar lines, golfers should concentrate on twisting exercises that help to maintain proper form during the golf swing.
If your pain persists for several weeks or more, you may build up scar tissue in the area. A successful treatment to break up scar tissue and promote healing is the Graston Technique.

Graston Technique for Golfer's Elbow in Chandler
Graston technique is one of the best ways to break up scar tissue that develops in chronic injuries to reduce pain and speed up healing. Graston technique utilizes stainless steel tools designed to break up the scar tissue by sheer force. When the tools slide along the skin they pull one layer of tissue past the other. The scar tissue is pulled apart, triggering the body's healing mechanisms to repair the fibers.
Cold Laser Technique For Tendons
Class IV cold laser or low level laser therapy is an excellent modality for decreasing pain and inflammation from golfer's elbow. Specific wavelengths and frequencies shut off the inflammatory cells, to decrease inflammation in the area. Different wavelengths and frequencies help to turn on repair and healing processes inside the cells. These wavelengths speed up the delivery of adenosine triphosphate (ATP), which is "fuel" for the cells created from the blood sugar your body makes from food.The repairing cells use this energy to lay down healthy fibers more quickly, reducing pain and speeding up the healing process.

Hand and Wrist Exercises
Many individuals with golfer's elbow develop weakness in the hands and wrists because of tendonosis of the flexor muscles. Hand and wrist exercises will help to strengthen these muscles and resolve muscle imbalances that may have developed between the flexor, extensor, pronator and supinator muscles in the forearm, hand or wrist.
Many of these exercises are easy to do at home with minimal equipment. For more information refer to our section on elbow, hand and wrist exercises.
Shockwave Therapy
Extracorporeal shockwave therapy uses a percussive instrument to break up fascial adhesions and scar tissue in the injured area. It is an effective way to enhance range of motion and decrease pain.
Shockwave therapy accelerates tendon healing and repair. It also causes the breakdown of scar tissue adhesions and conversion to proper tendon collagen. The treatment utilizes the body's natural healing and repair processes by causing micro damage to scar tissue and areas with chronic tendinopathy.

Shockwave therapy causes a very fast compression on the tissue, which effectively "stomps on the tissue." The sudden impact stretches the less flexible scar tissue and breaks it, triggering proper tissue repair. It produces a peak pressure over 1,000 times that of ultrasound waves to stimulate tissue repair and break up scar tissue. It is a very different treatment than ultrasound.
The treatment is not painful - much more comfortable than other treatments such as Graston Technique, ASTYM, or IASTM. These treatments also trigger tendon repair by activating the body's same tissue repair systems. Except Graston Technique and ASTYM utilize shearing and pulling across the scar tissue to tear it, which can cause bruising and excessive inflammation.
Watch The Video Below on Shockwave Therapy For Injuries
All of the treatments can help with tendon repair. We often use Graston Technique and shockwave therapy together to treat injuries. Shockwave therapy is commonly used first on very tender or painful injuries because it is more comfortably applied and produces less bruising and inflammatory response.
The intensity of shockwave therapy can be increased or decreased to make sure it is always comfortable. It should not hurt. Patients are often surprised that the comfortable compression can trigger the body's healing response. Those being treated with neck and back injuries frequently feel immediate relief and improved range of motion.
Many of our older patients prefer shockwave therapy to more aggressive soft tissue treatments because it causes less bruising and soreness post treatment, especially for those on blood thinners.
Why Did The Tendon Become Damaged?
Tendinopathy is pain and reduced function of tendons. Often the injury is due to the culmination of multiple pathological processes rather than a single event. The chronic repetitive stress leads to loss of tissue integrity and subsequent tearing or rupture.
I like to compare chronic repetitive injuries as adding pennies to a penny jar. Some days you add 15 pennies, some days you take out five pennies. Over time there is a tendency to add more pennies than you are removing, and eventually the jar starts to overflow. The overflowing penny jar is your chronic repetitive stress injury. There was not a single event or day that filled the jar; instead, the jar became full after an accumulation of days and pennies.

Often people are adding pennies to their jar because of muscle weakness, fatigue, or injury in other parts of their body. In addition to removing existing pennies from the jar, treatment will focus on reducing the amount of pennies you are adding every day.
The amount of repetitive stress placed upon your body can be dramatically reduced by changing postures and habits. For example, a person with low back pain may be uncomfortable sitting, which causes him to slouch at the computer. The slouching was contributing to neck pain and headaches. Improving the lower back pain will allow a person to sit with better posture and thus strain the neck less during the day.
Damage To Tendons
Mechanical and physical stress on tendons pull on the fibers. Too much pulling causes tears in the fibers, or even "fraying." Tendons will try and heal and repair, but cannot always completely finish repairing before the next trauma or physical stress.
Most Achilles tendon ruptures occur when participating in sporting activities. Often the ruptures are low grade damage has occurred. Biopsies have shown chronic degenerative changes in most ruptured Achilles tendons. These cases could be classified as acute trauma of chronically degenerated tendons.
In simple terms, the Achilles tendon has been chronically irritated with repetitive activity that has not completely healed, and then the Achilles ruptures during activity with a specific incident.

Repetitive loading and activity can be detrimental to tendon structures. The tendon repair mechanisms do not have enough time to heal before the onset of the next microtrauma or physical stress. This leads to a compromised tendon that is more susceptive to rupture.
Internal or intrinsic factors can make an individual more or less likely to suffer from a tendon injury. Factors include age, sex, and disease, such as diabetes, rheumatoid arthritis, ore genetic predisposition. Your overall health and condition can alter tendon structures or your ability to heal.
Muscle And Tendon Structure
The anatomical structure of muscles is like a licorice pull-and-peel. One fiber is wrapped in a group of fibers called a fascicle. Each fascicle is wrapped in a group of fascicles to form a muscle bundle. All the fibers are wrapped in coverings called fascia.
The coverings wrap around the individual fiber and the entire bundle. Each of the fascial coverings are a potential source of scar tissue formation, which will limit how the fiber slides and moves. This also changes the stress and strain that the muscle can handle.

This is the tendon, which is completely made of fascia and does not have any contractile properties like muscle. The muscles and fibers eventually end in a tendon that attaches to the bone. The muscle fascial coverings become thickened and dense before they attach to the bone.
Muscle contraction causes joint movement by pulling one bone closer to the other. Tendons transmit the forces produced by the muscles to the bone. The tendon is like a big thick rope; the tendon fibers are all aligned in the same direction to absorb the pulling forces.
Tendon fibers are made of type I collagen. This is a thick fiber designed to absorb and transmit forces. Excessive stress and strain in the fibers cause damage. Microtears in tendons are like nicking the fibers with a razor blade which cuts the fiber or causes it to fray. The body will try and repair this damage with proper type I collagen or it will form a temporary scar tissue patch with type III collagen.
In addition to chronic repetitive stress, microtears can be caused by uneven force production that results in uneven tendon loading. The amount of force absorbed by the tendon and the uneven distribution of forces lead to micro trauma and repair.

What are Scar Tissue And Fascial Adhesions?
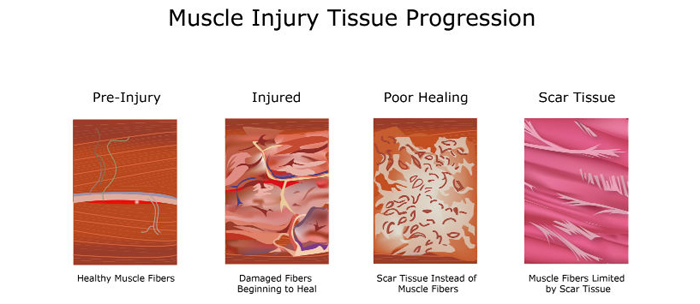
Scar tissue forms when tissue does not heal correctly, or is under chronic repetitive stress. Scar tissue is weaker than normal muscle and connective tissue, which is why it becomes chronically sore with activity.
Scar tissue is like the body's duct tape; it is meant as a short term patch to help support tissue. However, in some cases the scar tissue is not replaced with normal type I collagen fibers. Instead, a weaker type III collagen is used as the duct tape.
Fascial adhesions are another term for scar tissue. Adhesions cause restrictions between the body's fascia. Stiffness, loss of normal range of motion and chronic pain develops from the type III collagen patches of fascial adhesions.
The next time a scar tissue patch undergoes stress and strain, it becomes aggravated and flares up. This process causes more scar tissue to be added to the outside of the patch and the process repeats itself over and over, leading to larger accumulation of scar tissue patches.
I like to describe these larger scar tissue patches as "onions." Scar tissue ends up growing in layers around the initial injury. Stress to the area aggravates the outside layers and triggers another layer to be formed. The layers further from the center are easier to aggravate than the inside layers, which is why the onion continues to grow in size without causing the inside area to properly repair.
Think of a chronic injury or area that bothers you. The same weak spot always flares up, whether it is in your low back, neck, or knee. The pain always seems to start in the same place over the years. This source of continued pain is a "scar tissue onion" or weak spot that keeps flaring up.
Causes of Scar Tissue
Four Common Causes of Scar Tissue
- Trauma- Sudden accident. Injuries like stepping off a curb or falling off a ladder.
- Repetitive Motion Injury- Same motion over and over.
- Improper Mechanics- Slouching at a computer makes muscles work harder to hold up your head, neck, and shoulders.
- Aging- Years of wear and tear on the body adds up.
In the end, any scar tissue that limits movement and causes pain needs to be broken up to restore normal motion.
That was the simple version.
A more complex and histological description of tendinopathy would include decreased oxygen and blood flow to the injured area. Tissue oxidative stress further decreases tissue repair and increases inflammatory cytokines. Tenocytes can produce substance P, catecholamines, glutamate, and acetylcholine.
Additional tissue repair cells play a role in tendon repair. Tenocytes within the tendon and sheath activate healing. Neutrophils and macrophages play a role in removing tissue debris and release chemicals that lead to the next phase of tissue repair.
The weaker scar tissue patch is made of type III collagen. In an ideal situation, the next repair phase transitions the type III to type I collagen, and this can continue for years beyond the original injury.

Is One Therapy Better Than Another For Chronic Tendinopathy?
No single therapy is consistently more effective than others. Sorry!
Multiple therapies are often required for chronic tendinopathy repair and healing. We utilize shockwave therapy, Graston Technique, and class IV low level laser therapy to enhance tissue repair. Proper treatment and rehabilitation of tendinopathy injuries often requires incorporating exercises and stretches to increase muscle flexibility and strength. Then teaching the body how to use those muscles again properly. Muscle pattern and joint stability exercises can help prevent future injuries.
Our Chandler Chiropractic and Physical Therapy clinic treats patients with a variety of muscle, tendon, joint and ligament injuries. The clinic provides treatment for endurance athletes and weekend warriors in addition to common headache, neck and back patients traditionally seen in Chiropractic, Physical Therapy, Massage Therapy clinics. We work with all ages and abilities of the residents of Ahwatukee, Phoenix, Tempe, Gilbert, Mesa and Chandler AZ.